Imagine you knew the day, place and exact time you were going to die. Bearspaw resident Hugh Wallace knew he would die on April 19, 2016 in his family home at 5 p.m.
Imagine you knew the day, place and exact time you were going to die.
Bearspaw resident Hugh Wallace knew he would die on April 19, 2016 in his family home at 5 p.m.
The 75-year-old requested a doctor-assisted death after living more than two decades with multiple sclerosis (MS) and a more recent diagnosis of small-cell aggressive lung cancer.
“Hugh said, ‘I do not want to extend my dying, if you can extend my living that would be great' but he could see in the cards that it was not possible, ” said Evie Wallace, Hugh's widow.
Less than a year after Hugh's death, Evie is now an outspoken advocate for medically assisted death and has been bringing Hugh's story across Southern Alberta.
“I feel so strongly about being able to choose and I saw how positive of an experience it was for our family, ” Evie explained over coffee.
“To see someone suffer is god awful and to leave, with some dignity of who you are, is beautiful. ”
The Supreme Court of Canada unanimously ruled Canadians have the right to medically assisted death under certain situations in February 2015 but Bill C-14 legislation on medical assistance in dying did not receive royal assent until June 17, 2016 - more than two months after Hugh died.
“It is not for everyone, ” Evie said.
Hugh battled his cancer with radiation and managed the pain with medication, including fentanyl, before he made the decision in March 2016 that he was ready to die.
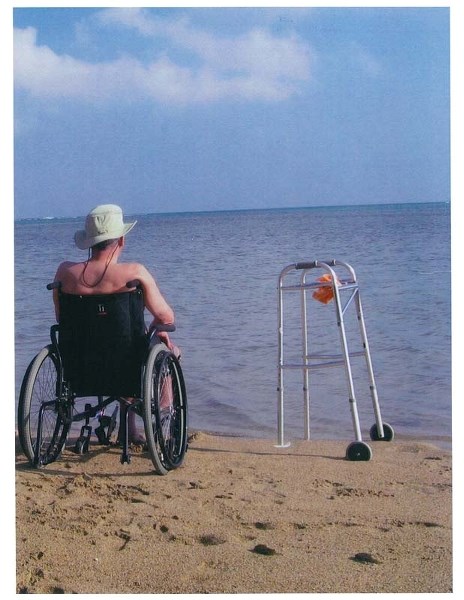
Known for his curiosity and love, Hugh was described as a person with a “zeal for life ” with stories of a dogsledding journey with limited mobility, being lumped in a wheelbarrow to make off-beaten areas accessible and winching himself off a sailboat in the South Pacific to enjoy the beauty of a coral reef.
“Hugh always said if it ever came to a point when he couldn't open his own beer then to shoot him - he was a very pragmatic, scientific man, ” Evie said.
The process of obtaining a doctor-assisted death before June was not an easy road, the widow explained.
Two physicians performed a medical competency test where the Bearspaw resident explained his death was foreseeable and that he was in pain psychologically, mentally and physically. Hugh, Evie, the couple's children, Hugh's sister and nephew all had to go to write letters explaining their relationship with Hugh and how they felt about his decision and then go to court.
The judge approved the application on April 15 and after finding a pharmacy to administer the lethal dosage, Hugh and his family were informed “death would happen on a Tuesday. ”
“Knowing that my husband is going to die on a specific day, at a specific time in his own bed at five o'clock - I can't even tell you how anxiety provoking that is, ” Evie said.
“That being said, we never infantilized him, we never made him out to be the sick person. ”
Hugh died on April 19, and was the first person in Alberta to die by medically assisted death.
Now, 10 months after Hugh's death and more than five decades of marriage, three children and eight grandchildren, Evie wants to share their family's story to get people to “start talking. ”
“One of our close friends said what Hugh did was selfish - it is very easy to call the game from the bleachers - but I thought what Hugh did was the most generous, selfless act, ” Evie said.
To date, 92 people in the province have died with medical assistance since Feb. 6, 2016, according to Alberta Health Services. Out of the 92 deaths in the province, 26 people were in the Calgary Zone and 11 were in the southern Alberta zone.
“Though there are flaws in its approach, Alberta should be lauded for being proactive about the implementation of assisted dying in the province. Unlike other provincial and territorial governments, Alberta didn't wait until after the federal legislation was passed to implement regulations that offer clarity to patients and their physicians, ” said Cory Ruf, communications co-ordinator for Dying with Dignity Canada.
“We're relieved that Bill C-14 gives dying Canadians the option to die in peace with the help of a physician. However, the legislation does not comply with the Supreme Court's 2015 decision on assisted dying because it discriminates against Canadians on the basis of their diagnoses. ”
The most cited health conditions of those who have died with a doctor-assisted death in Alberta are cancer, multiple sclerosis (MS) and amyotrophic lateral sclerosis (ALS) and according to Alberta Health Services, 48 applications for medical assisted death have been denied due to ineligibility reasons including, mental health diagnosis, loss of capacity or competency, and death that is not reasonably foreseeable.
“It's clear that dying Canadians who are suffering intolerably and want the choice of assisted dying available to them face numerous barriers to access, particularly in small towns and remote communities, ” Ruf said.
“Publicly funded hospitals that refuse to allow assisted dying - or even assessments for assisted dying - on-site, a shortage of physicians who are participating in the practice, and healthcare facilities that have not yet issued policies for assisted dying are examples of factors that impose confusion and create delays for patients who are looking to questions answered. ”
Dying with Dignity is currently crowd sourcing the Shine a Light campaign to uncover the barriers that “prevent Canadians who want to access their right to assisted dying. ”
Until then, the process to access death with medical assistance in Alberta consists of meeting a checklist of eligibility requirements. Those include being of legal age, 18 years or older, passing an assessment from provincial physicians, having have a grievous and irremediable medical condition, having the capacity to provide informed consent and providing written and signed consent.
“The cycle of life, Hugh understood it. This is probably for very few people but it's about choice, ” Evie explained.
“No one is saying you have to go this road. ”
For more information on medical assisted death in Alberta, go to albertahealthservices.ca.
FACTBOX
When filling out the record of request for medical assistance in dying, a person, who is an adult of at least 18 years of age and capable of making decisions in respect to their health, must sign their initials in a box of requirements that reads;
“I believe, and a medical practitioner or a nurse practitioner has informed me, that I have a grievous and irremediable medical condition and that all of the following apply:
- I have a serious and incurable illness, disease or disability;
- I am in an advanced state of irreversible decline in capability;
- My illness, disease or disability or state of decline causes me enduring physical or psychological suffering that is intolerable to me and cannot be relieved under conditions that I consider acceptable;
- My natural death has become reasonably foreseeable, taking into account all of medical circumstances.